Gestational diabetes mellitus occurs with the onset of pregnancy and is characterized by the inability of the pregnant patient to tolerate glucose. Patients who develop gestational diabetes may develop diabetes later in life. However, gestational diabetes often resolves after delivery. The cause of gestational diabetes is largely unknown.
Gestational Diabetes Mellitus Risk Factors
Factors that place patients at risk for developing gestational diabetes mellitus include:
• Maternal obesity
• Advanced maternal age
• Gestational diabetes in previous pregnancies
• History of previous baby with high birth weight
• History of spontaneous abortion
• Family history of diabetes mellitus
Gestational Diabetes Mellitus: Maternal and Foetal Complications
A variety of maternal and foetal complications are associated with gestational diabetes mellitus.
• Significant chance of delivering via caesarean section due to the large size of infants born to patients with gestational diabetes.
• Increased frequency of hypertension.
• Infants born to patients with gestational diabetes mellitus are usually macrosomic (high birth weight >4.5 kg). This occurs due to the condition that stimulates excessive growth. These large infants may have difficulty manoeuvering the birth canal, and a caesarean section may be required. If vaginal delivery is attempted, the infant is at risk for shoulder dystocia or other birth injuries.
• After delivery, the newborn infant’s blood glucose must be monitored regularly due to the sharp decrease in available glucose after the umbilical cord is cut. The newborn’s pancreas continues to produce insulin after delivery despite the decrease in serum glucose. This adds to the potential instability of the infant’s blood glucose.
Gestational Diabetes Mellitus Treatment
Pregnant patients are routinely screened for gestational diabetes mellitus between 24 and 29 weeks’ gestation.
1. Most patients with gestational diabetes are treated through diet. They are encouraged to consume a proper diet and obtain adequate safe exercise.
2. Some patients may require insulin or oral hypoglycemia agents to manage gestational diabetes mellitus.
3. Resistance exercise can help overweight patients with gestational diabetes avoid insulin therapy.
4. A referral to a dietician may also be necessary.
5. During labour, the patient with gestational diabetes mellitus may need to be on intravenous insulin and glucose. Blood glucose levels will be monitored regularly according to medical history.
6. After delivery, there will be monitoring of the infant’s blood glucose levels, as glucose instability is common in newborns born to patients with gestational diabetes mellitus. If the newborn’s blood glucose level is below acceptable levels, treatment with intravenous fluids, intravenous or oral glucose, or early feedings is necessary.
7. Note the signs and symptoms of hypoglycaemia (low sugar) which include shakiness, anxiety, headache, hunger, cold, clammy skin, and tingling around the mouth and see the healthcare practitioner immediately if signs and symptoms are noted.
8. Hypoglycemia in women is treated by immediately eating 10 to 20 g of a mixed protein and carbohydrate snack. This mixed protein and carbohydrate snack tends to dampen the rapid elevation of glucose followed by a rapid decline that can result in pregnant women with diabetes from consuming a pure simple sugar.
9. Since the potential for developing diabetes is significant in patients with gestational diabetes, it is important that patients understand the need for follow-up evaluation after delivery. Patients should continue to watch for signs and symptoms of hypoglycemia and notify their healthcare practitioner if seen.
PRETERM LABOR AND BIRTH
Preterm labour refers to labour that occurs after 20 weeks’ but before 37 weeks’ gestation. Preterm birth, a consequence of preterm labour, refers to delivery prior to 37 weeks’ gestation.
Risk Factors
Preterm birth is a significant contributor to infant mortality rates. A variety of risk factors predispose patients to preterm labour and subsequent birth.
• Infection
• Dehydration
• Premature breaking of the waters
• Uterine bleeding
• Diabetes
• Substance abuse
• Smoking
• Incompetent cervix
• Multiple gestations
• Preeclampsia
• Poor nutrition
• Poverty (e.g., homelessness, low socioeconomic status)
• History of preterm labour and birth
• Young or advanced maternal age
• Maternal Injury e.g. accidental falls, physical abuse etc
Gestational Diabetes Mellitus Maternal and Foetal Implications
The mother may suffer from stress due to the diagnosis of preterm labour and birth as well as from the causative agent. Specifically, patients may be experiencing preterm labour and birth due to conditions such as sepsis. The foetus is at great risk for delivering early as a result of preterm labour. The effects of preterm labour and birth depend on the gestational age of the foetus at delivery. However, the immaturity of foetal lungs in the presence of preterm labour and birth is a significant concern.
Gestational Diabetes Mellitus: Signs and Symptoms
• Feeling of pressure in the pelvic area.
• Abdominal and/or uterine cramping or contraction.
• Painful or painless contractions.
• Constant back pain.
• Amniotic membranes may rupture prematurely; therefore a sudden gush or constant trickle of vaginal fluid may be noted.
Gestational Diabetes Mellitus: Treatment
1. Medical treatment for preterm labour and birth is dependent upon the gestational age of the foetus. Generally, healthcare practitioners seek to avoid delivery of patients prior to 34 weeks gestation to allow further maturation of the foetal lungs.
2. They often prescribe antibiotics to treat infection, glucocorticoids to increase foetal lung maturity, intravenous therapy to maintain hydration, and tocolytics to control uterine contractions in patients with preterm labour.
3. Vital signs, contractions, and foetal status will be closely monitored when patients are faced with the possibility of delivering a preterm infant.
4. Avoid activities that may disturb the cervix and cause labour or infection (e.g., vaginal exams, sexual activity, orgasm, tampons, douches)
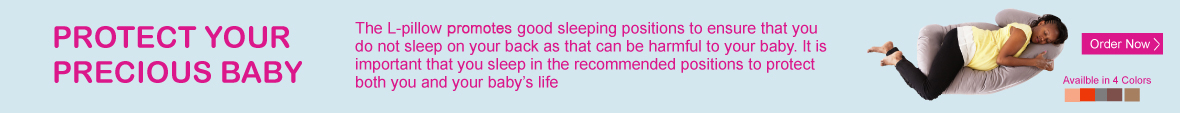
5. Rest in the side-lying position to improve blood flow to the uterus.
6. Consume adequate fluid to prevent dehydration, which causes the release of oxytocin.
7. Notify their healthcare practitioner immediately if any of the following signs and symptoms are noted: uterine contractions, cramping or irritability, constant back pain, a gush or a constant trickle of vaginal fluid or fever.